Type 1 vs Type 2 Diabetes- 15 Minutes to Read
What is Diabetes?
- What is Diabetes?
- Types of Diabetes:
- Type 1 vs Type 2 Diabetes Signs and Symptoms:
- Type 1 vs Type 2 Diabetes Treatment:
- Medicines for Type 1 vs Type 2 Diabetes:
- How to diagnose Type 1 vs Type 2 Diabetes?
- Can you have Type 1 and Type 2 Diabetes at the same time?
- How to test for Type 1 vs Type 2 Diabetes?
- What happens in both Type 1 vs Type 2 Diabetes?
- Which is Worse Between Both Type1 and Type2 Diabetes?
- Type 1 vs Type 2 Diabetes: Which type of Diabetes is worse for Covid?
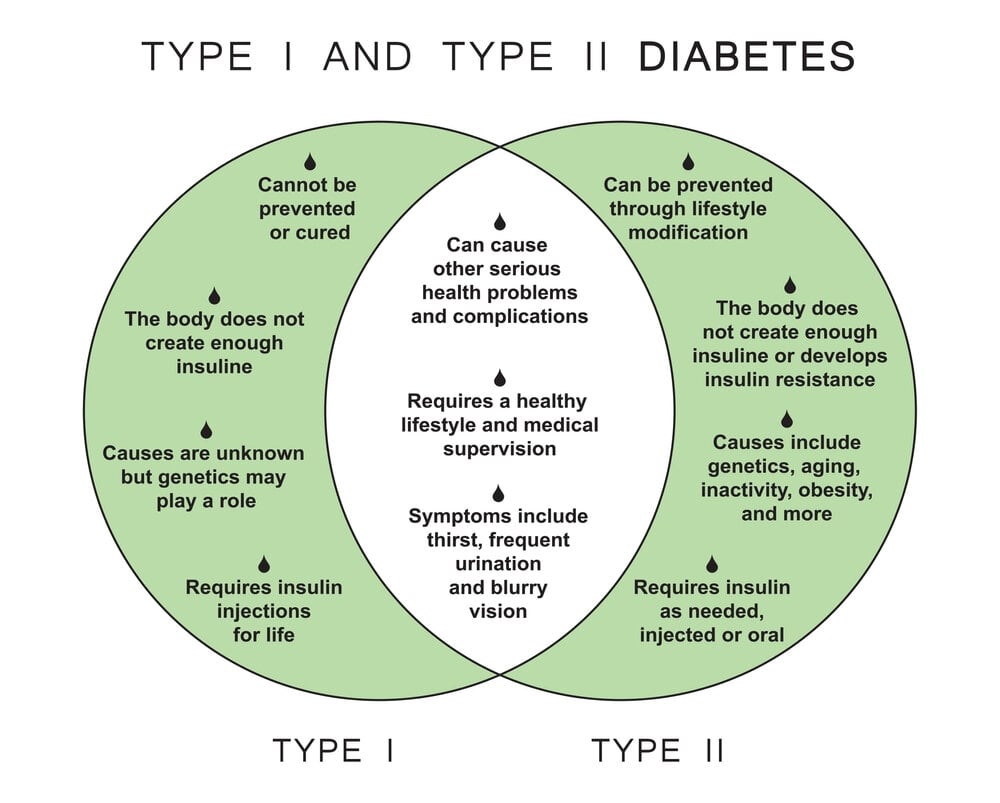
- Can Type 1 or Type 2 Diabetes be cured or prevented?
- End Note:
- Take-Home Message:
The way your body converts food into energy is affected by diabetes, a chronic (long-lasting) health disease. Let’s understand Type 1 vs Type 2 Diabetes in detail.
The majority of the food you consume is converted to sugar, commonly known as glucose, and then released into your bloodstream. The pancreas is prompted to release insulin when the blood sugar levels rise. For blood sugar to enter the body’s cells and be used as energy, insulin functions as a key.
If a person has diabetes, the body either produces insufficient insulin or is unable to utilize it as effectively as it should. Too much blood sugar remains in the bloodstream when there is insufficient insulin or when cells stop responding to insulin.
That can eventually lead to major health issues like renal disease, eyesight loss, and heart disease which constitute signs and symptoms of Type 1 vs Type 2 Diabetes.
Although there is currently no treatment for diabetes, decreasing weight, eating well, and exercising can all be very beneficial. Taking medicine as needed, getting diabetes self-management education and support, and keeping health care appointments can also lessen the burden of diabetes on your life.

Although there is currently no treatment for diabetes, decreasing weight, eating well, and exercising can all be very beneficial. Taking medicine as needed, getting diabetes self-management education and support, and keeping health care appointments can also lessen the burden of diabetes on your life.
Types of Diabetes:
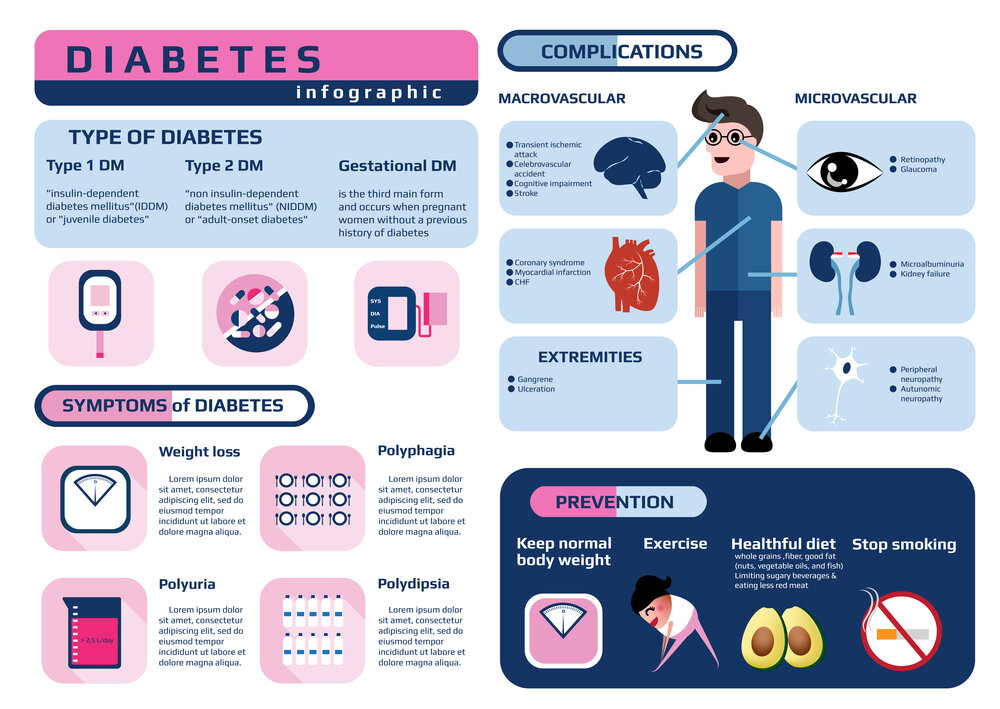
There are Three Basic Forms of Diabetes: Type 1, Type 2, and Gestational Diabetes (Diabetes while Pregnant). Know about Type 1 vs Type 2 Diabetes vs Gestational Diabetes.
Type 1 Diabetes:
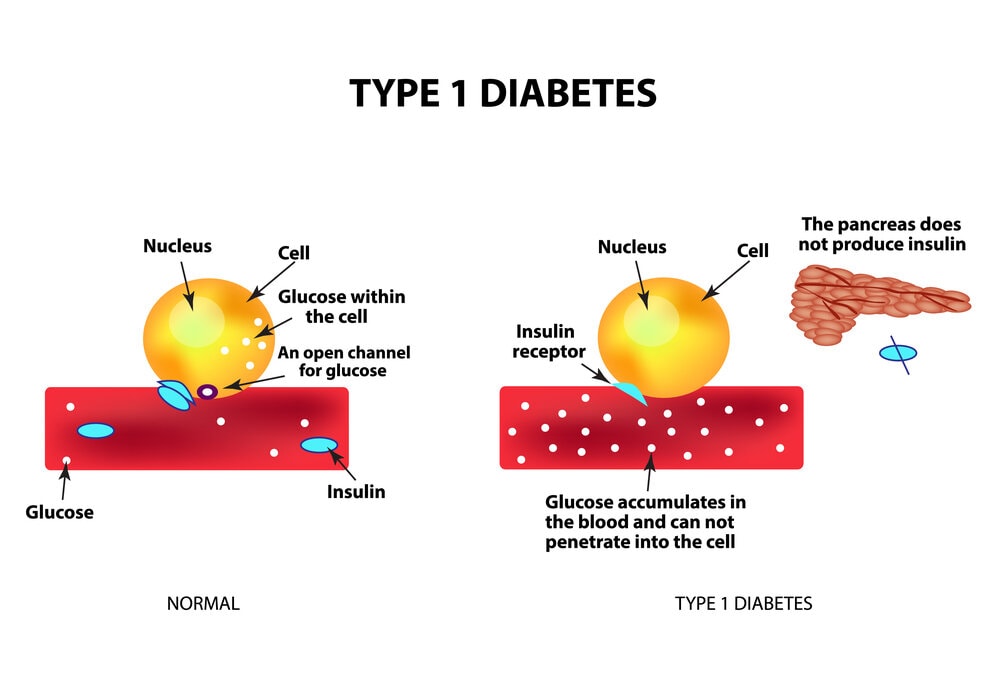
Type 1 Diabetes is believed to be brought on by an autoimmune reaction, in which the body unintentionally attacks itself and prevents the production of insulin. Type 1 diabetes affects roughly 5 to 10 percent of those who have it.
Type 1 diabetes symptoms frequently appear suddenly. Children, teenagers, and young adults are typically diagnosed with it. You must take insulin every day to stay alive if you have type 1 diabetes. There is currently no cure for type 1 diabetes.
Type 2 Diabetes:
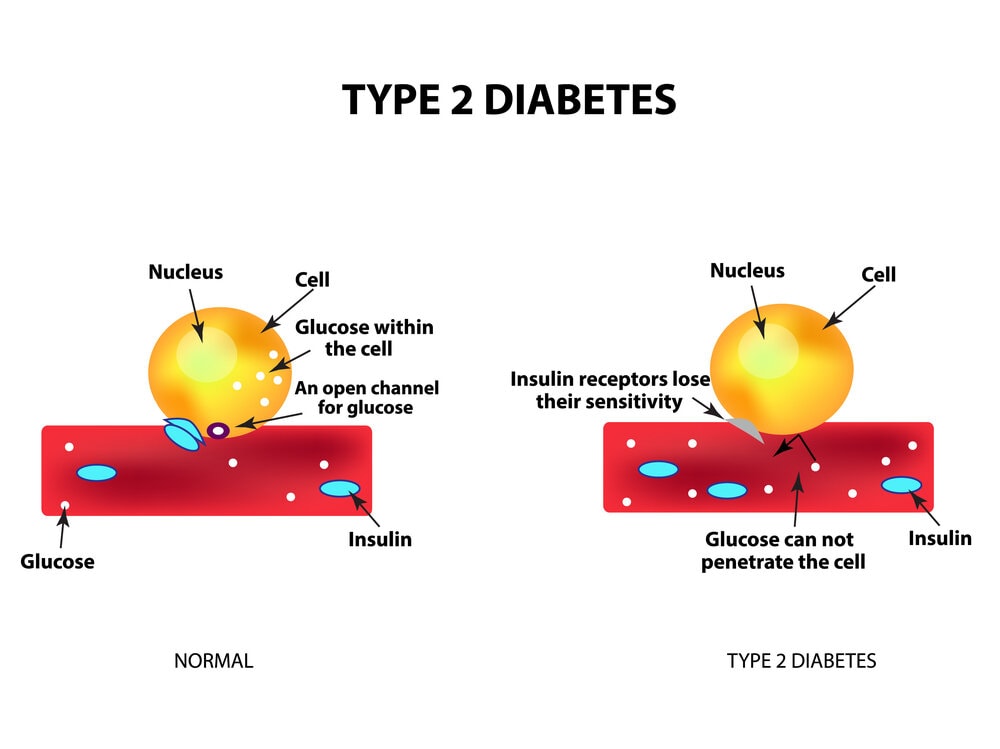
The body struggles to properly utilize insulin in type 2 diabetes, making it difficult to maintain normal blood sugar levels. Type 2 diabetes affects 90–95% of patients with diabetes. It takes years to develop, and adults are typically diagnosed with it (but more and more in children, teens, and young adults).
If a person is at risk, it is crucial to have the blood sugar tested because he/she might not exhibit any symptoms. With healthy lifestyle modifications like weight loss, a nutritious diet, and regular exercise, type 2 diabetes can be avoided or postponed.
Gestational Diabetes:
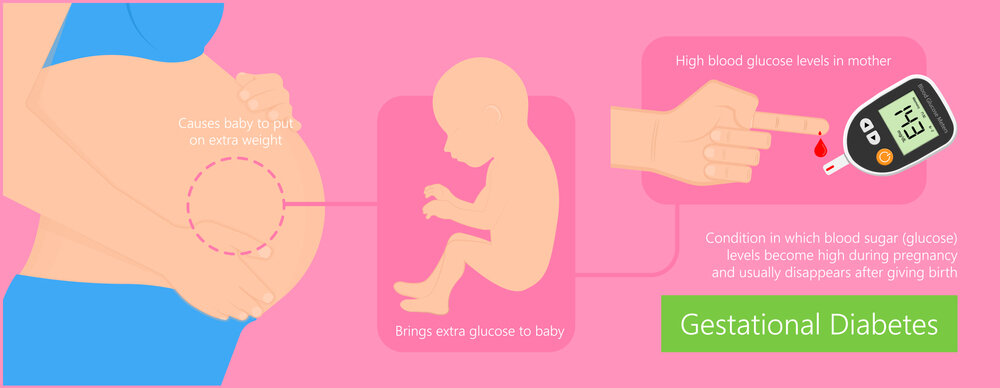
Women who have never had diabetes before and who become pregnant can acquire gestational diabetes. The kid may be more susceptible to health issues if the mother has gestational diabetes.
Although gestational diabetes often disappears after childbirth, it raises the chance of developing type 2 diabetes in the future. The child is more likely to be obese as a youngster or adolescent and to acquire type 2 diabetes in the future.
Type 1 vs Type 2 Diabetes Signs and Symptoms:
Type 1 Diabetes is a genetic illness that frequently manifests in childhood, but Type 2 Diabetes is primarily connected to lifestyle choices and develops over time. The immune system attacks and kills the insulin-producing cells in the pancreas when a person has type 1 diabetes.
Type 1 Diabetes Signs and Symptoms:
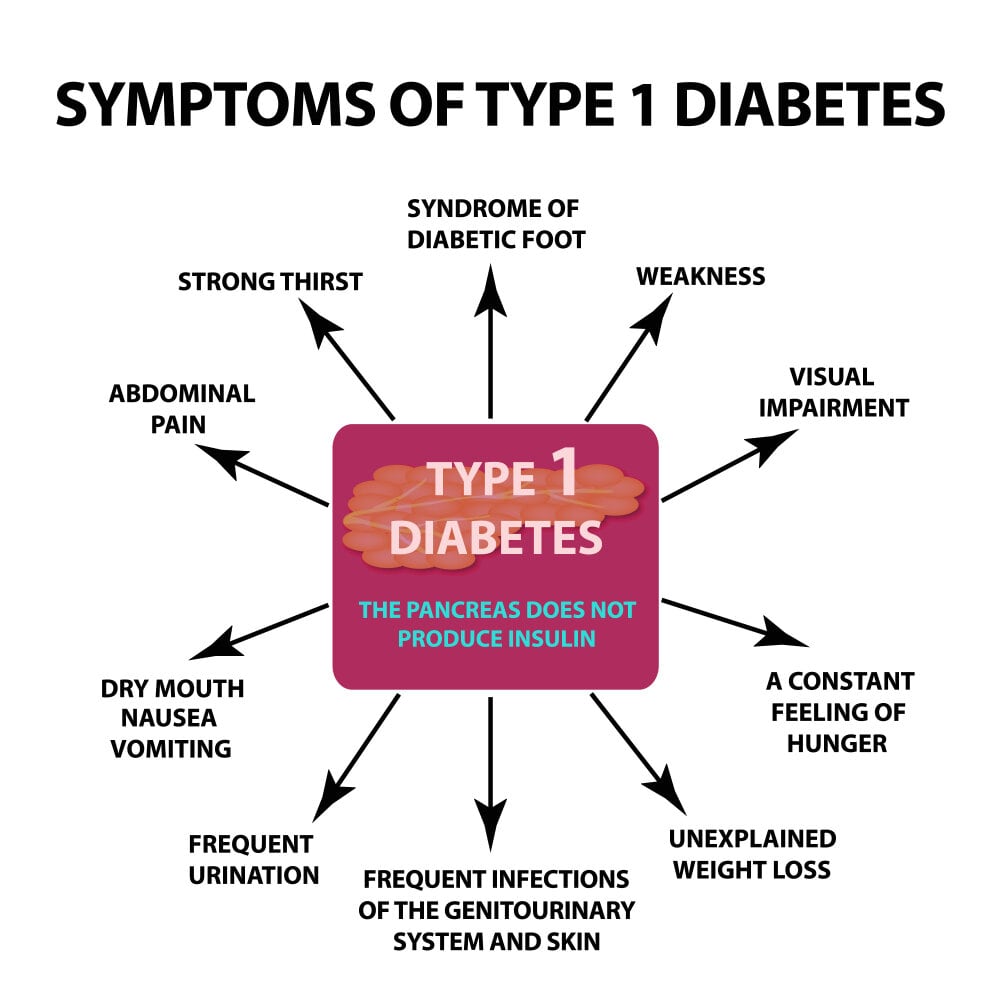
Signs and symptoms of Type 1 diabetes can occur suddenly and include:
- Increased thirst
- Frequent urination
- Bed-wetting in children who previously didn’t wet the bed during the night
- Extreme hunger
- Unintended weight loss
- Irritability and other mood changes
- Fatigue and weakness
- Blurred vision
Type 2 Diabetes Signs and Symptoms:
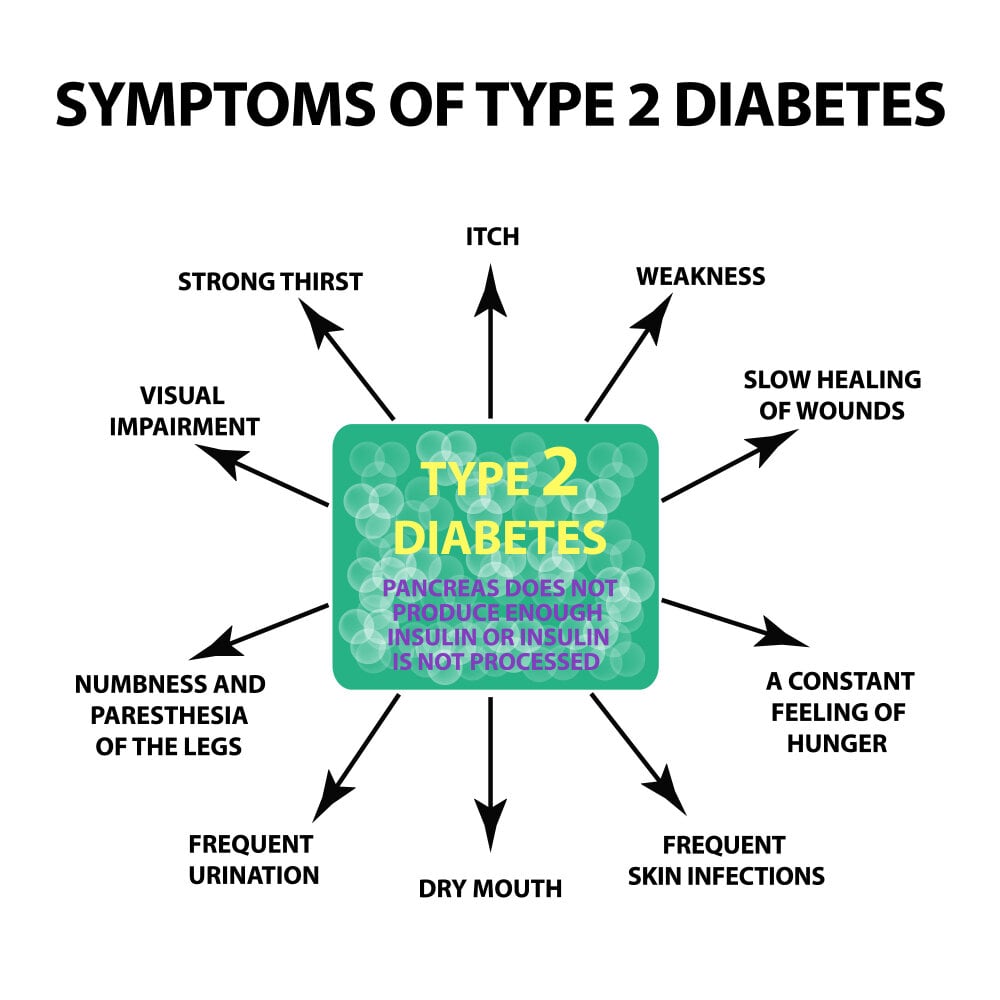
Type 2 Diabetes symptoms and signs frequently appear gradually. You may have Type 2 diabetes for years without realizing it. When present, signs, and symptoms may include:
- Increased thirst
- Frequent urination
- Increased hunger
- Unintended weight loss
- Fatigue
- Blurred vision
- Slow-healing sores
- Frequent infections
- Numbness or tingling in the hands or feet
- Areas of darkened skin, usually in the armpits and neck
Type 1 vs Type 2 Diabetes Treatment:
Type 1 Diabetes is treated with:

- Injecting insulin
- Protein, fat, and carbohydrate counts
- Regular monitoring of blood sugar
- Eating nutritious food/a balanced diet
- Maintaining a healthy weight and doing regular exercise
To delay or avoid issues, a patient wants to keep his or her blood sugar level as close to normal.
In general, the person wants to keep the blood sugar levels during the day, before meals, between 80 and 130 mg/dL (4.44 to 7.2 mmol/L) and 180 mg/dL (10 mmol/L), two hours after eating.
Type 2 Diabetes Management Entails:
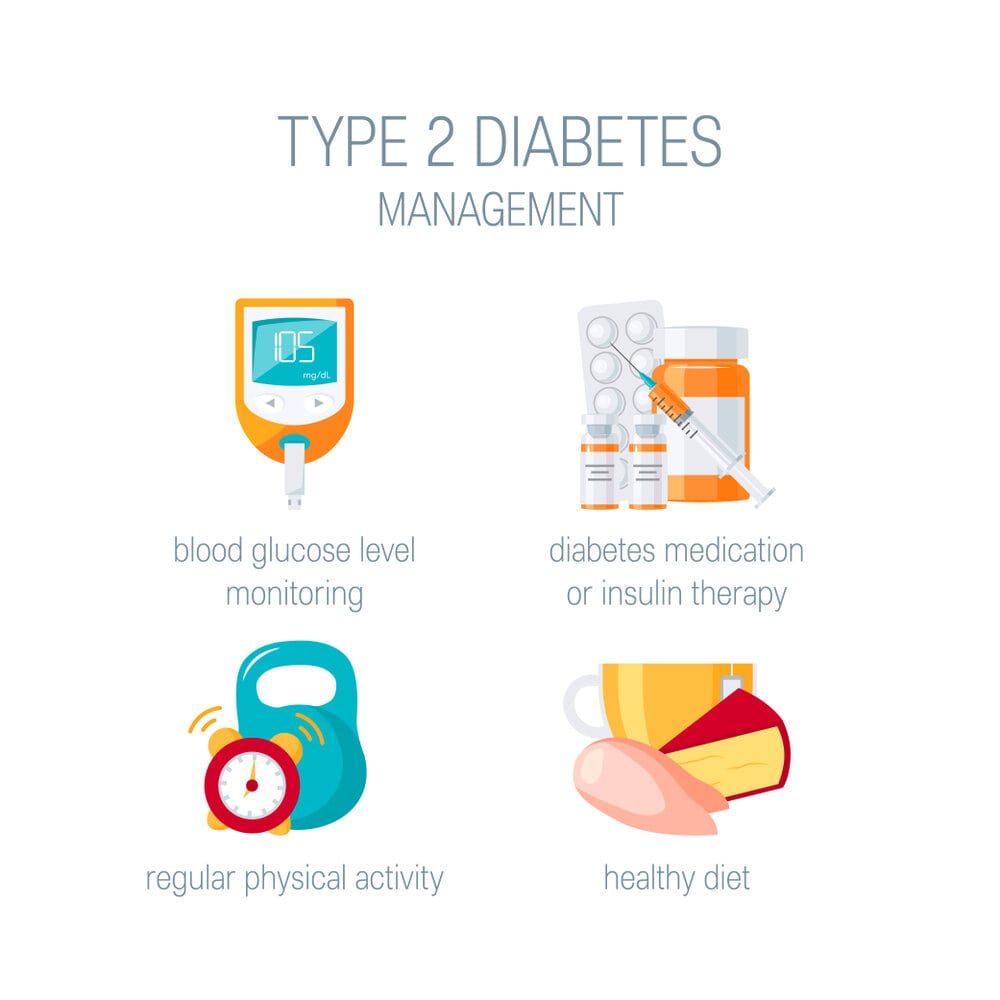
- Optimum nutrition/ balanced diet
- Routine exercise
- Losing weight
- Insulin treatment or diabetes medicines
- Monitoring blood sugar
By taking these actions, you can assist in maintaining your blood sugar levels near normal levels, which can help delay or stop issues.
Medicines for Type 1 vs Type 2 Diabetes:
Medicines for Type 1 Diabetes:

Type 1 Diabetics require lifetime insulin therapy. There are numerous insulin subtypes, including:
- Short-acting (regular) insulin
- Rapid-acting insulin
- Intermediate-acting (NPH) insulin
- Long-acting insulin
Because stomach enzymes will break down the insulin and stop it from working, insulin cannot be given orally to reduce blood sugar. It must be administered to the patient either intravenously or with an insulin pump.
Medicines for high blood pressure. To support the health of your kidneys, your doctor might recommend ACE inhibitors or ARBs—angiotensin II receptor blockers. Patients with diabetes who have blood pressures greater than 140/90 millimeters of mercury are advised to take these drugs (mm Hg).
Aspirin: After discussing the potential risk of bleeding with you, your doctor may advise you to take a baby or regular Aspirin every day to protect your heart if they believe you have an elevated risk for a cardiovascular event.
Medicines that reduce cholesterol. Due to the increased risk of heart disease, cholesterol recommendations for those with diabetes tend to be more stringent.
Insulin Dosage administration with either insulin Injections or Pumps.
Diabetes Type 2 Medicines:
The doctor may recommend insulin therapy or diabetic drugs that lower insulin levels if a person is unable to maintain their target blood sugar level with diet and exercise. The following are some drug therapies for type 2 diabetes:
The first treatment for diabetes type 2 is typically Metformin. It works by reducing liver glucose synthesis and enhancing insulin sensitivity so that the body utilizes insulin more efficiently.
Your body produces more insulin when you use Sulfonylureas. Glyburide (DiaBeta, Glynase), glipizide (Glucotrol), and glimepiride are other examples (Amaryl).
The pancreas is induced to secrete more insulin by Glinides. They work more quickly than sulfonylureas and have a shorter effect on the body.
The body’s tissues become more responsive to insulin when given Thiazolidinediones. Examples include Pioglitazone and Rosiglitazone (Avandia) (Actos).
DPP-4 inhibitors lower blood sugar levels, however, their impact is typically extremely small. Examples include Linagliptin, Sitagliptin, and Saxagliptin (Januvia, Onglyza) (Tradjenta).
Injectable drugs known as GLP-1 receptor agonists assist reduce blood sugar levels by slowing digestion. Some of them may lower the risk of heart attack and stroke, and their use is frequently linked to weight loss.
Insulin therapy is necessary for some type 2 diabetics. Nowadays, if blood sugar targets aren’t achieved with lifestyle changes and other drugs, insulin therapy may be administered sooner rather than later.
How to diagnose Type 1 vs Type 2 Diabetes?
Let’s know some procedures on how to diagnose Type 1 vs Type 2 Diabetes.
The A1C, or glycated hemoglobin test, is the main procedure used to identify both Type 1 and Type 2 diabetes. Your average blood sugar level over the previous two to three months is determined by this blood test. Your doctor might prick your finger or take a sample of your blood.
The A1C level will be higher the higher blood sugar levels have been during the preceding few months. Percentages are used to represent test results. Diabetes is identified by an A1C score of 6.5 percent or higher. For those who have sickle cell anemia or the sickle cell trait, the A1C test is inaccurate.
The doctor will need to do a different test if the patient has this ailment or characteristic.
Can you have Type 1 and Type 2 Diabetes at the same time?
Although Type 1 and Type 2 Diabetes are not typically diagnosed at the same time, patients with Type 1 diabetes may eventually show signs of Type 2 diabetes.
An autoimmune disorder called Type 1 diabetes causes the body to stop producing insulin. When a person has Type 2 diabetes, their body can still manufacture some insulin, but not enough, and they have poor insulin utilization.
Chronically elevated blood glucose levels result from this. Insulin resistance is the term used to describe a condition in which the body uses insulin less and less effectively over time.
Despite the underlying differences between the two disorders, type 1 diabetes sufferers can nevertheless develop an inability to effectively use prescribed insulin, reflecting some of the symptoms of type 2 diabetes. Because of a disorder called metabolic syndrome, this frequently occurs.
According to studies, most persons with type 2 diabetes also have metabolic syndrome. Additionally, even those with type 1 diabetes can have metabolic syndrome, which can result in insulin resistance and other type 2 traits.
Although some specialists argue that the description “those with type 1 diabetes who also have type 2 traits” is more appropriate, this occurrence is commonly referred to as “Double Diabetes.”
How to test for Type 1 vs Type 2 Diabetes?

Type 1 Diabetes:
A1C test for glycated hemoglobin: Your average blood sugar level over the previous two to three months is determined by this blood test. It calculates the proportion of blood sugar bonded to the protein that carries oxygen in red blood cells (hemoglobin).
Random test for blood sugar: A random blood sample will be drawn, and subsequent testing might confirm the results.
Millimoles per liter (mmol/L) or milligrams per deciliter (mg/dL) are used to express blood sugar levels. No matter when you last ate, having a random blood sugar level of 200 mg/dL (11.1 mmol/L) or higher suggests diabetes, especially if it is accompanied by any of the telltale symptoms, like extreme thirst and frequent urination.
Blood sugar test after fasting: After an overnight fast, a blood sample will be collected. It is normal to have a fasting blood sugar level of less than 100 mg/dL (5.6 mmol/L). Prediabetes is defined as having a fasting blood sugar level between 100 and 125 mg/dL (5.6 and 6.9 mmol/L). You have diabetes if it is 126 mg/dL (7 mmol/L) or above on two different tests.
Type 2 Diabetes:
The Glycated Hemoglobin (A1C) test is typically used to identify type 2 diabetes. Your average blood sugar level over the previous two to three months is determined by this blood test. This is how the results are interpreted:
- Normal is less than 5.7 percent.
- Prediabetes is a condition that affects 5.7 to 6.4 percent of people.
- Diabetes is identified by two independent tests yielding a 6.5 percent or greater.
Your doctor may use the following tests to diagnose diabetes if the A1C test isn’t available or if you have specific conditions that interfere with an A1C test:
Random test for blood sugar: Millimoles of sugar per liter (mmol/L) of blood or milligrams of sugar per deciliter (mg/dL) are used to express blood sugar levels. No matter when you last ate, a level of 200 mg/dL (11.1 mmol/L) or above indicates diabetes, particularly if you also exhibit symptoms of diabetes like severe thirst and frequent urination.
Blood sugar test after fasting: After fasting for the previous night, blood is drawn. This is how the results are interpreted:
- Normal ranges are below 100 mg/dL (5.6 mmol/L).
- Diagnosis of prediabetes ranges from 100 to 125 mg/dL (5.6 to 6.9 mmol/L).
- Diabetes is identified when two different tests show 126 mg/dL (7 mmol/L) or above.
Test for oral glucose tolerance: Except during pregnancy, this test is less frequently utilized than the others. You must abstain from food for the entire night before drinking a sweet beverage in the doctor’s office. For the following two hours, blood sugar levels are checked at regular intervals. This is how the results are interpreted:
- A normal level is less than 140 mg/dL (7.8 mmol/L).
- Prediabetes is defined as a blood sugar level of 140 to 199 mg/dL (7.8 and 11.0 mmol/L).
- After two hours, a 200 mg/dL (11.1 mmol/L) or higher level suggests diabetes.
Screening: All adults age 45 and older, as well as the following groups, should undergo routine testing for type 2 diabetes with diagnostic tests:
- Individuals under 45 who are overweight or obese and have one or more diabetes risk factors
- Pregnant women with gestational diabetes
- Those with prediabetes who have received a diagnosis
- Children who are overweight or obese, have a history of type 2 diabetes in their family, or who otherwise pose a risk.
What happens in both Type 1 vs Type 2 Diabetes?
Let’s understand what happens in both Type 1 vs Type Diabetes:
Diabetes Type 2 is not the same as diabetes Type 1. Your pancreas doesn’t produce any insulin if you have Type 1 diabetes. In Type 2, your pancreas produces insufficient insulin, and the insulin that does get produced isn’t always effective. Both kinds are diabetes mellitus subtypes that result in hyperglycemia (high blood sugar).
Although it is increasingly prevalent among adolescents, Type 2 diabetes typically affects older persons. Although persons of any age can develop Type 1 diabetes, it typically first manifests in childhood or young adults.
Which is Worse Between Both Type1 and Type2 Diabetes?
Type 1 vs Type 2 Diabetes, Which is worse!!
If diabetes is not properly diagnosed or controlled, both Type 1 and Type 2 can have very dangerous side effects. Both must be treated seriously. Either type of diabetes increases the risk of heart disease, stroke, blindness, blood vessel and nerve damage, and kidney failure if it is not properly treated.
There is no superior or inferior one. Both illnesses need to be managed with caution and awareness. Your cells will start to die if they do not receive the sugar they require to function.
It’s harmful to have too much or too little blood sugar, especially for your brain. To prevent unconsciousness, organ damage, and other catastrophic problems, it’s critical to control your insulin and sugar levels.
Both kinds of diabetes have shorter life expectancies. People with type 2 diabetes may experience a life expectancy reduction of roughly 10 years, whereas type 1 diabetics may experience a life expectancy reduction of more than 20 years.
Type 1 vs Type 2 Diabetes: Which type of Diabetes is worse for Covid?

Regarding COVID-19, one thing to keep in mind is that we still have a lot to learn. We do know that patients with diabetes appear to experience more severe COVID-19 disease development.
Not that persons with diabetes are more likely to get COVID, but when they do, the condition is far more severe and seems to advance more quickly. Both type 2 and type 1 diabetes appear to be prone to, a more severe form of the disease, however, type 1 patient may fare better due to their earlier age.
According to the CDC’s current information, type 1 or gestational diabetes may raise a person’s chance of developing a serious illness from COVID-19. We don’t understand how underlying medical disorders enhance the risk for severe sickness from COVID-19 as well as we’d like to because it’s a novel disease.
The majority of the body’s insulin-producing cells are killed by an immunological reaction in people with type 1 diabetes. The environment—in the sense of increased food intake, decreased physical activity, and increased weight—interacts with their family history, which gives the genes, to cause type 2 diabetes, as does genetic susceptibility.
More inflammation occurs in the body in diabetic patients. Therefore, one cause could be that the inflammatory condition worsens considerably more quickly with COVID.
The second reason is that those who have diabetes may be more susceptible to circulatory issues. They may have already undergone a bypass, suffered a stroke, or experienced reduced blood supply to the legs, among other things.
After that, this happened since there is now an additional circulation problem on top of previous circulatory problems. COVID-19 may increase blood flow brought by clotting issues. Therefore, lesser justifications may be nested within each of these larger ones.
It’s critical to keep in mind that individuals with any kind of diabetes can differ in age, the number of complications they have had, and their level of diabetes management.
Regardless of the kind of diabetes they have, persons who already have health issues related to diabetes are more likely to experience worse outcomes if they catch COVID-19 than people with diabetes who are otherwise healthy.
Can Type 1 or Type 2 Diabetes be cured or prevented?

Although there is no known cure for diabetes, it can be managed, and in rare cases, remission can occur. You must take the following actions to effectively manage diabetes:
Maintain control over your blood sugar. Know what to do each day to help keep them as close to normal as you can: Regularly monitor your blood glucose levels. Regularly take your diabetes medication.
In addition, maintain a healthy balance and natural remedies for diabetes between your food consumption and your medicine (diabetes medicine jardiance), exercise, stress relief, and sleep schedule.
Each meal should be prepared. As much as you can, follow your diabetes meal plan.
Bring along some wholesome snacks. You won’t be as prone to graze on empty calories.
Regular exercise keeps you in shape, burns calories, and helps keep your blood sugar levels normal.
Keep all of your scheduled medical appointments. Included in this are your physician, diabetes educator, ophthalmologist, dentist, podiatrist, and other medical specialists.
End Note:

Unfortunately, neither Type 1 nor Type 2 diabetes are currently permanently curable.
However, there is proof that some Type 2 diabetics can go into remission by decreasing weight. You can put Type 2 diabetes into remission by having surgery, eating a very low-calorie diet while under a doctor’s care, or both.
In order to improve treatment and care, we are also supporting certain crucial research projects. A remedy for both Type 1 and Type 2 diabetes is also needed.
Take-Home Message:
Some forms of diabetes, such as Type 1, are brought on by external sources. Better eating choices, more exercise, and weight loss help prevent some diseases, such as Type 2 Diabetes.
Talk to your doctor about the potential hazards of Type 1 vs Type 2 Diabetes. Have your blood sugar checked if you’re at risk, and then manage your blood sugar according to your doctor’s recommendations.
Related Article:

